Glossary of Terms – Vein, Diagnosis and Treatment Terms
Find answers to your questions about vein disease and treatment options.
Leg Vein Anatomy
The leg venous system comprises a network of veins, including:
- Superficial venous system: Veins located close to the surface of the skin. There are two principal vessels in the superficial venous system:
- Great saphenous vein (GSV): A large superficial leg vein running from the front of the anklebone, traveling alongside the inside of the leg and thigh until it empties into the deep vein in the groin called the femoral vein.
- Small saphenous vein: A superficial leg vein that runs from outside of the foot and travels up the back of the calf where it empties into the deep vein in the crease of the knee (popliteal vein).
- Deep veins: Larger veins located deep in the muscles of the leg.
- Perforator veins: Veins that connect the superficial veins to the deep veins. The perforator veins are like the rungs on the ladder of the leg venous system.
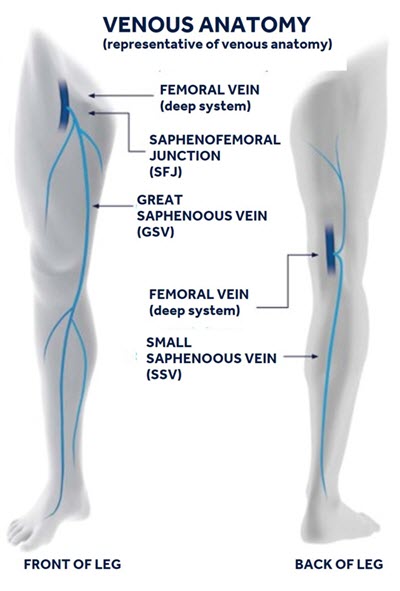
A front and back view of the venous anatomy of the legs.
Varicose Veins
Veins in the leg that become swollen and have disease or damaged valves are known as varicose veins. Veins can become varicose when the vein valves that regulate the direction of blood flow become damaged or diseased, weaken and no longer function properly. Instead of blood moving toward the heart like it should, blood stays in place and pools in the vein of the leg.
Spider Veins
Often covering the legs, these damaged veins appear to be similar to varicose veins, only thinner. Often red or blue in color and appearing like thin spider webs or branches, these veins are closer to the skin surface and can spread; however, unlike varicose veins, spider veins are typically not raised above the skin’s surface. Spider veins can be treated with sclerotherapy or laser treatment. Though spider veins may be associated with varicose veins or CVI, the issue is seen as cosmetic and treatment is generally regarded as elective.
Vein Valve
Healthy leg veins contain valves, or small delicate flaps of tissue that open and close to help regulate blood flow to the heart. These veins are designed to allow blood to flow against gravity from the legs back up toward the heart. The valves help control the flow of blood to make this happen. With age and other stresses on the body, these valves can weaken and lose the ability to regulate the direction of blood circulation.
Venous Reflux
Venous reflux is the term that describes what happens when the valves in the veins grow weak or damaged and lose the ability to regulate the direction of blood flow. When blood “leaks” down past a bad valve, it is called reflux. Reflux causes blood to pool in the leg veins as opposed to moving upward toward the heart.
Ulcer
If CVI is left untreated, legs can sometimes develop painful sores or wounds on the skin’s surface called ulcers. Ulcers may indicate a more severe and progressive state of the disease. Normally ulcers appear near the ankles or lower leg and are brought on from the increased build-up of fluid and blood pressure from veins affected by CVI.
How quickly can I resume normal activity?
Patients treated with the ClosureFast procedure may resume normal activities more quickly than patients who undergo surgical vein stripping or laser ablation. With the ClosureFast procedure, the average patient typically resumes normal activities within a few days. For a few weeks following the treatment, the doctor may recommend a regular walking regimen and suggest you refrain from very strenuous activities (heavy lifting, for example) or prolonged periods of standing.
How soon after treatment will my symptoms improve?
Most patients report relief of symptoms after two days with a noticeable improvement in one to two weeks.
Is there any scarring, bruising, or swelling after the procedure?
Most patients report limited to no scarring, bruising, or swelling following the ClosureFast procedure using the ClosureFast catheter.
How is the ClosureFast procedure different from endovenous laser?
Although the ClosureFast procedure and 980 nm endovenous laser ablation are both minimally invasive procedures, a comparative, multi-center study showed that the ClosureFast procedure was associated with statistically significant lower rates of pain, bruising, and complications. Patients undergoing the ClosureFast procedure also reported improvements in quality of life measures up to four times faster than patients treated with 980 nm endovenous laser ablation.
How is the ClosureFast procedure different from vein stripping?
During vein stripping, incisions are made in the groin and calf, and a tool is threaded through the diseased vein to pull the vein out of the leg. With the ClosureFast procedure, only one small incision is made at the insertion site and the vein is then treated and left in place. This minimally invasive approach reduces the likelihood of pain and bruising associated with vein stripping surgery.
Is the ClosureFast procedure covered by insurance?
Many insurance companies pay for the ClosureFast procedure in part or in full. The ClosureFast procedure has coverage policies with major health insurers. Please discuss your coverage with your insurance provider or our office.
What does it treat?
The VenaSeal closure system treats symptomatic vein disease in the lower extremity superficial truncal veins, often the underlying cause of painful varicose veins.
What can I expect of the VenaSeal procedure?
Before the Procedure:
You will have an ultrasound imaging exam of the leg that is to be treated. This exam is important for assessing the diseased superficial vein and planning the procedure.
During the Procedure:
Your doctor can discuss the procedure with you. A brief summary of what to expect is below:
- You may feel some minor pain or stinging with a needle stick to numb the site where the doctor will access your vein.
- Once the area is numb, your doctor will insert the catheter (i.e., a small hollow tube) into your leg. You may feel some pressure from the placement of the catheter.
- The catheter will be placed in specific areas along the diseased vein to deliver small amounts of the medical adhesive. You may feel some mild sensation of pulling. Ultrasound will be used during the procedure to guide and position the catheter.
- After treatment, the catheter is removed and a small adhesive bandage placed over the puncture site.
After the Procedure:
- You will be taken to the recovery area to rest.
- Your doctor will recommend follow-up care as needed.
When will my symptoms improve?
Symptoms are caused by the diseased superficial vein. Thus, symptoms may improve as soon as the diseased vein is closed.
When can I return to normal activity?
The VenaSeal procedure is designed to reduce recovery time. Many patients return to normal activity immediately after the procedure. Your doctor can help you determine when you can return to normal activity.
Is the VenaSeal procedure painful?
Most patients feel little, if any, pain during the outpatient procedure.
Is there bruising after the VenaSeal procedure?
Most patients report little-to-no bruising after the VenaSeal procedure.
What happens to the VenaSeal adhesive?
Only a very small amount of VenaSeal adhesive is used to close the vein. Your body will naturally create scar tissue around the adhesive over time to keep the vessel permanently closed.
How does the VenaSeal procedure differ from thermal energy procedures?
The VenaSeal procedure uses an adhesive to close the superficial vein. Thermal energy procedures use heat to close the vein. The intense heat requires a large volume of numbing medicine, which is injected through many needle sticks. The injections may cause pain and bruising after the procedure.
Is the VenaSeal procedure covered by insurance?
As with any procedure, insurance coverage may vary. For more information, please contact your insurance provider or call our office.